Expert Consensus on Diagnosis and Treatment of neonatal Mycoplasma pneumoniae pneumonia (2024) part II
III. Diagnosis of neonatal MPP
1. Comply with the clinical and imaging manifestations of neonatal pneumonia, the diagnosis of neonatal MPP can be combined with any of the following:
1) Peripheral blood MP-IgM antibody positive;
2) Positive MP-DNA or RNA in throat swabs or sputum;
3) Positive MP antigen in throat swab or sputum;
4) Positive MP culture.
2. Meeting the diagnostic criteria of MPP, one of the following conditions was considered as neonatal severe MPP:
1) Respiratory rate ≥70 times /min or apnea;
2) Lung smell and moist rales and/or signs of consolidation;
3) Lung imaging shows lung involvement ≥50% or accompanied by pleural effusion;
4) Blood gas analysis indicated respiratory failure;
5) Severe extrapulmonary complications that threaten life.
Recommendation 4:
During the epidemic period of MP, it is necessary to attach great importance to neonatal MPP, pay close attention to the changes in the condition of newborns meeting the diagnostic criteria of MPP, and identify severe MPP in time.
When a newborn is diagnosed with MPP and continues to have fever after formal treatment with macrolides for 72 h, with no improvement or further aggravation of clinical signs and lung imaging, in addition to being alert to non-responsive MPP and refractory MPP, other bacterial, viral and fungal infections should also be considered. It is recommended to improve the relevant detection in time. And give the appropriate treatment.
Ⅳ. Treatment of neonatal MPP
Although the incidence of MPP in newborns is relatively low, persistent fever and worsening of clinical symptoms may still occur, respiratory failure or life-threateningextrapulmonary complications may occur. Early treatment can reduce the probability and severity of sequelae of MP infection. Due to the lack of cell wall, MP is resistant to almost all β-lactam, sulfanilamide,trimethoprim, rifampicin and other drugs that act on bacterial cell wall. At present, there is no consensus at home and abroad on the selection, dosage and course of antibacterial drugs for neonatal MPP. Macrolides may be recognized as the first choice of therapeutic drugs.
Recommendation 5:
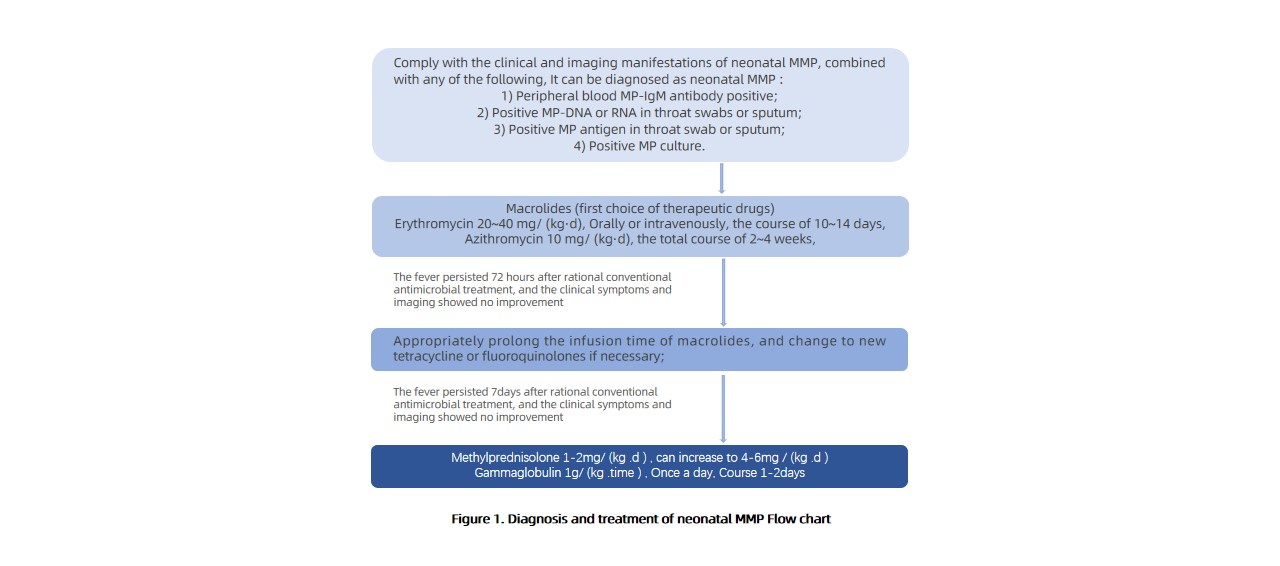
For the diagnosed MPP newborns should receive macrolides as soon as possible, the first choice is erythromycin 20~40 mg/ (kg·d), divided into 2~3 times, the course of 10~14 days, or azithromycin 10 mg/ (kg·d), once a day, the course of 3~4 days, if necessary, can be extended to 5~7 days. After an interval of 3~4 days, the second course of treatment began, the total course of 2~4 weeks, the initial treatment of severe cases or children who can not be fed orally or gastrointestinal absorption disorders choose intravenous preparations, and then changed to oral drug sequential treatment after the condition become stable.
Recommendation 6:
When there is non-responsive MPP or refractory MPP of macrolide drugs, the treatment plan should be adjusted according to the condition. With the informed consent of the guardian, new tetracycline drugs or fluoroquinolones can be selected if necessary. Meanwhile, drug sensitivity tests and electrocardiogram, liver and kidney function and immune function tests should be actively improved; When refractory MPP and severe MPP appear, glucocorticoid (methylprednisolone) or gamma globulin can be used as appropriate. Different treatment procedures should be taken according to the clinical severity of the child, as shown in Figure 1.
Ⅴ. Prevention of congenital MPP in neonates
Recommendation 7:
In view of the adverse maternal and infant outcomes after MP infection, attention should be paid to newborns born to MP-infected mothers, timely identification and judgment of MP-related detection, and timely initiation of targeted intervention measures based on test results and clinical judgment.
Ⅵ. Conclusion
The clinical manifestations of neonatal MPP are varied, and it is easy to be missed and misdiagnosed. Most mild MPP has a good prognosis, and if it develops into severe MPP, there is a higher complication rate and death risk. Reasonable examination means should be given as soon as possible for neonates suspected of MPP, and for children diagnosed with MPP, appropriate treatment plan should be selected according to the severity of the condition. To achieve early identification,early diagnosis and early treatment.